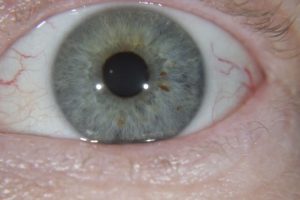
Iridology is the study of the iris, it is the coloured part of the eye that surrounds the pupil. It has been used as a health assessment tool for centuries by the ancient Greeks, Egyptians, Indians and the Chinese. Even today we will look at a person’s eyes and intuitively assess their life force – we talk about the life has gone out of their eyes, or their eyes were full of joy, Everyone’s eye is different.
The grandfather of current iridology is considered to be a Hungarian -. Ignatz Von Peczely (1822-1911). When Ignatz was 11 he saw a trapped owl in his backyard, As he set it free the owl broke its leg and at that instant Ignatz saw a line form in the owls eye. As the owl started to heal Ignatz observed the line disappearing and this sparked his interest in studying eyes and how they related to health.
Ignatz studied to become a medical doctor. He observed his patients, their symptoms and the markings he saw in their eyes, Through the correlations he created the first iridology map.
Since that time many refinements have been made and continue to be made to the iris map. The basis of the map is that each area of the iris is a reflex of a different area of the body, Changes in fibre structure or colour of the iris may reflect that that organ or system may require more support than other areas of the body.
A modern day iridologist will take a photo of your eye to assess what your iris will reveal. Being able to use magnification assists the iridologist in assessing what they see in the iris, and having a photo also makes it easier to show their findings to their client.
An iridology chart or map is used when looking at the iris to compare signs, pigments, colours and fibre distortion with where they correlate in the chart and what part of the body that section refers to.
The right iris reflects body organs and systems found in the right side of the body, and the left iris reflects body organs and systems found in the left side of the iris.
Iridology is a non-invasive diagnostic tool that requires no needles or drugs. In minutes iridology will bring to attention areas of your body that need support because of your genetic imprint. Personality or Rayid iridology will also give you great insight into your personality and coping mechanisms. Iridology will give insight into the level of inflammation in the body, the quality of the person’s digestion and elimination, and their inherent tissue strength. Through all this iridology can often reveal what areas need support when a client has unexplained symptoms. The insight gained through iridology can turn a person’s health around and allow them to be proactive in taking care of their bodies.
It is important to note that iridology does not determine your sex, if you are pregnant or your life span, it also doesn’t name or diagnose specific diseases.
Iridology looks at taking a holistic approach to help and not just the symptoms of a particular condition. eg. If you are prone to headaches, the iridologist will look at areas such as blood sugar and the pancreas, spine and muscles to check for alignment and tension, mucous and the lymphatic system to assess toxin removal and the nervous system and adrenal glands to assess stress load and identify which area(s) require the most attention.
Through using the iris map, iridology is able to identify systems or areas of the body that require support before they become serious issues giving the client the opportunity to be proactive in their health and take action to prevent the development of a disease or disorder.
Most iridologists will use a natural approach to any recommendations they make and this may include changes to what the person eats and their lifestyle, or the addition of nutrients, herbs, homeopathic remedies or flower essences to assist the healing process.
In conclusion iridology is the study of the iris of the eye to evaluate the person’s health on a physical and personality perspective. It is non -invasive and can give insight into why a person has symptoms or health issues. The iridologist may then recommend natural treatments based on what they have found to support the persons health and wellbeing.
Examples of a right and left iris below.